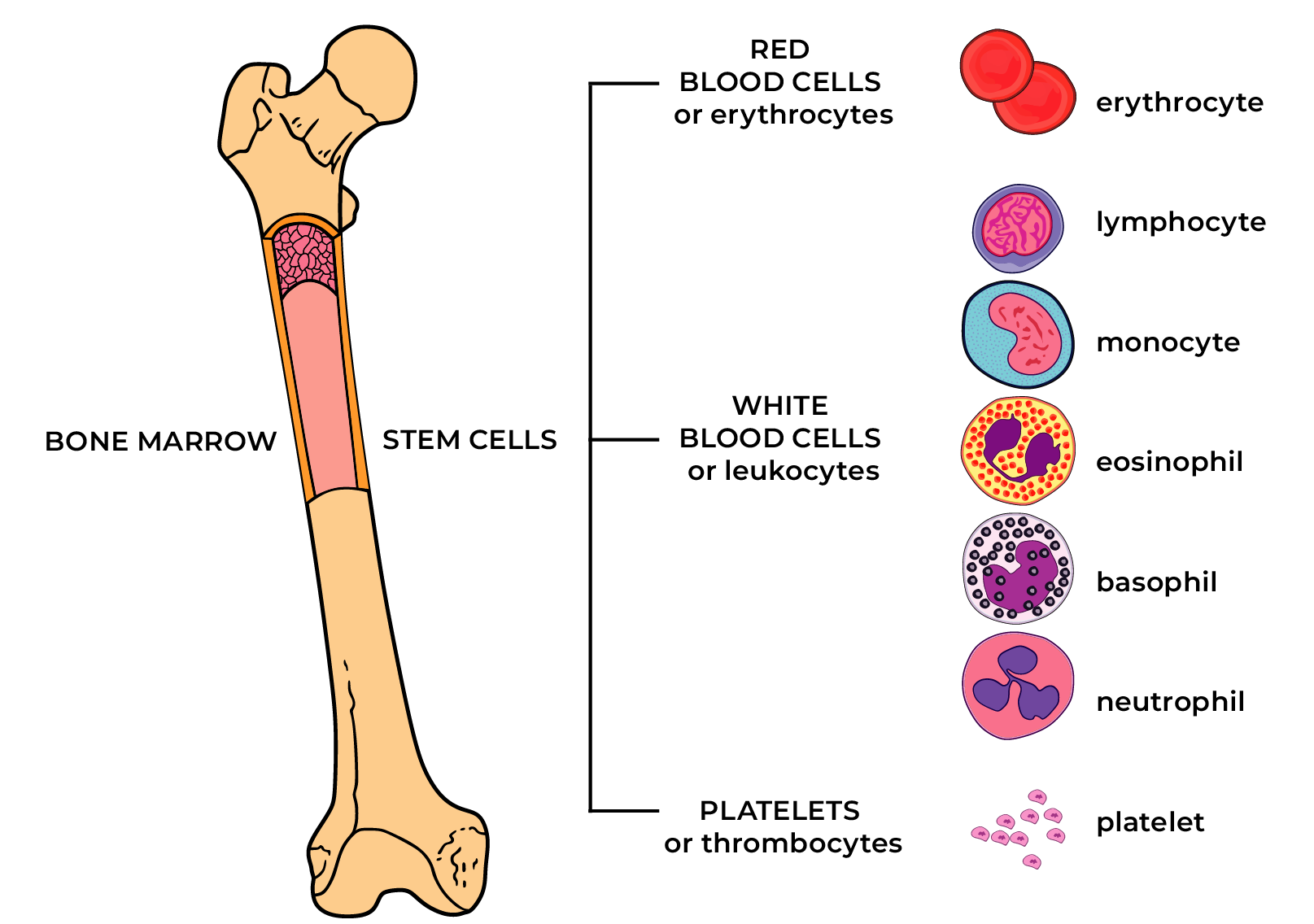
Essential thrombocythemia (ET) is a chronic hematopoietic system tumour, in the case of which too many platelets are produced in the bone marrow due to genetic changes in haematopoiesis. ET belongs to the group of myeloproliferative diseases. A thrombocyte or platelet is a very small blood cell with the task of participating in coagulation.
Essential thrombocythemia is characterised by:
- a higher than normal number of platelets (≥450 ~ 109/L) for at least two months when other causes of an increased number of platelets have been excluded;
- the development of disease-causing changes during life; and
- changes in blood count and bone marrow not characteristic to other haematopoietic diseases.
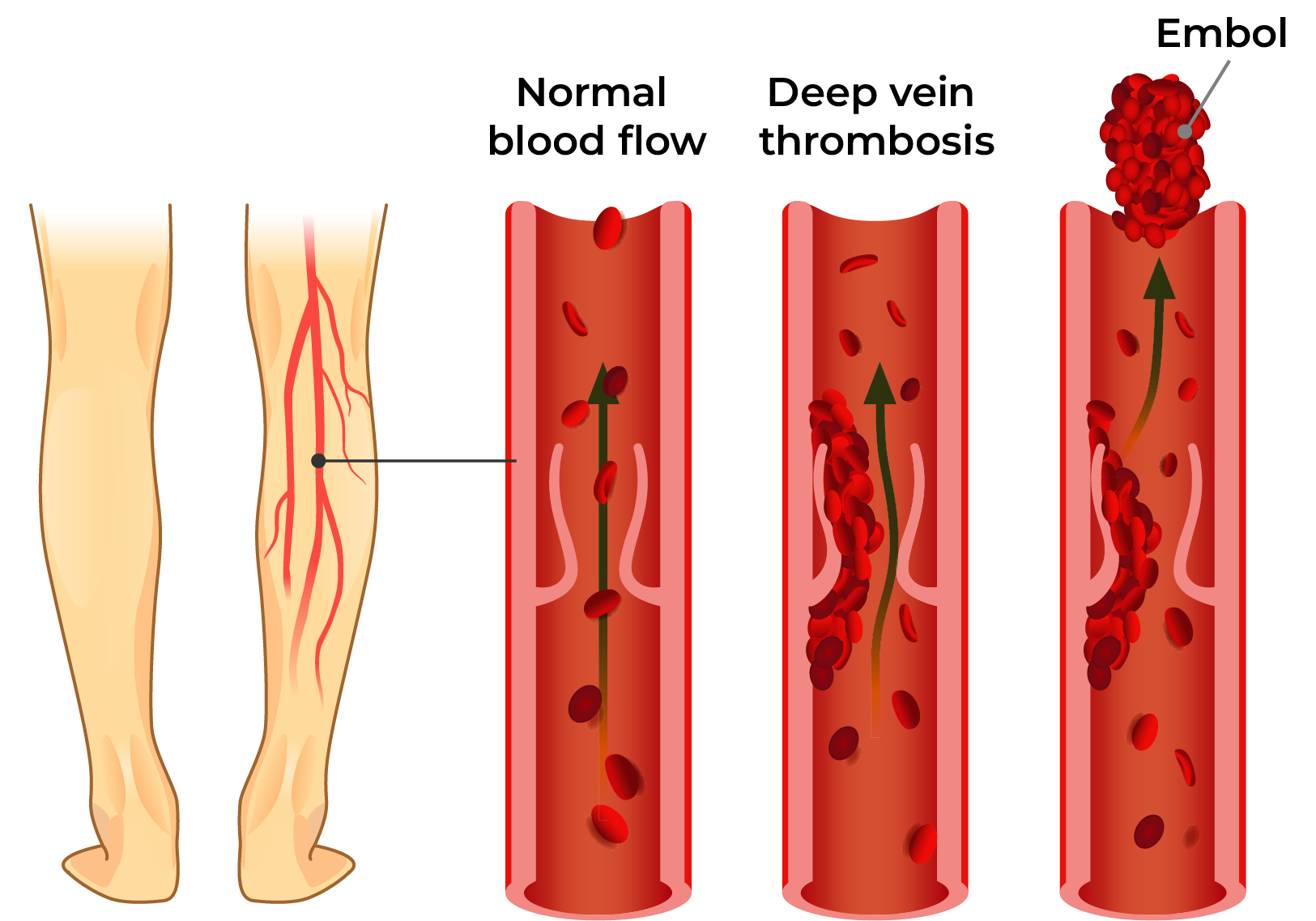
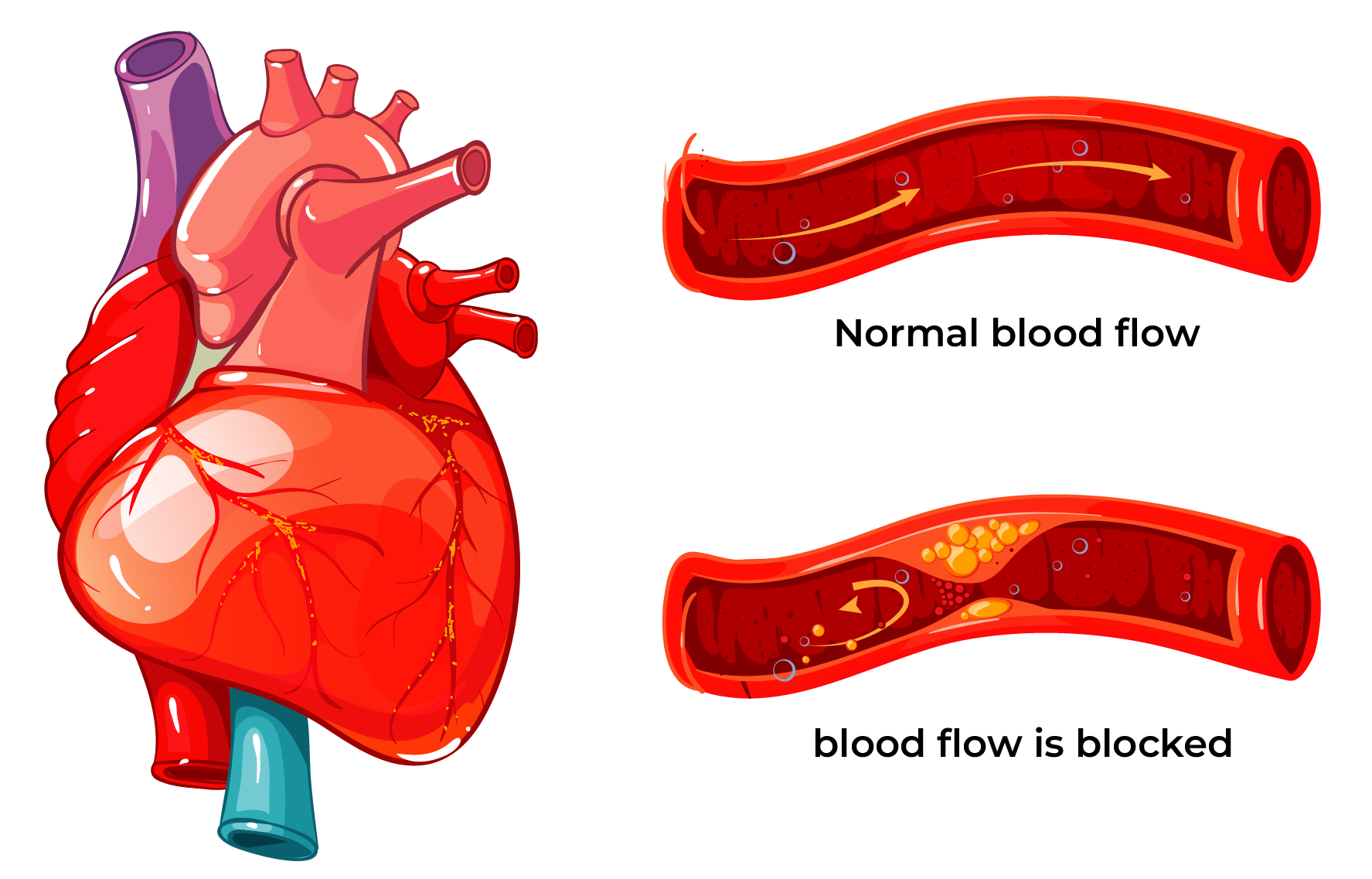
Where there is a very large number of platelets, thrombosis risk is increased because they may obstruct smaller blood vessels due to their large number. Less often, haemorrhages may occur because platelet function may be impaired with the increase in their number.
Venous thrombosis
Arterial thrombosis
The term ‘thrombocythemia’ describes an abundance of platelets in the blood. The term ‘essential’ indicates primary bone marrow disease, excluding other causes of platelet count increase, for example, infections, inflammatory diseases, operations, tumours, iron deficiency, absence of spleen. ET is a rare disease: around two new cases are diagnosed per 100,000 persons annually. Patients become ill mostly over the age of 60, but 20% of patients are less than 40 years old at the time of diagnosis. Among younger people, the percentage of women is bigger. Among older patients, the percentage of men and women is equal.
ET cannot be prevented and the causes of the disease are not yet completely understood. Most often, in around 60% of cases a change is found in the Janus-kinase 2 gene (JAK2) and in ROUND 30% of cases in the calreticulin gene (CALR). Less often, a change is found in the MPL gene with a similar mechanism of action. Gene changes are not found in 10-20% of patients and their impact on disease course and the resulting treatment options is still under scrutiny.
Symptoms
Many patients with ET diagnosis don’t have disease-related symptoms; increased platelet count in blood analysis is an accidental finding.
Possible symptoms:
- The signs of a transient disorder of cerebral blood supply or transitory ischaemic attack (TIA) may be headache, drowsiness, weakness, confusion, visual or speech disorder, etc. These symptoms occur due to the impairment of blood flow in the brain.
- Thrombosis is the main ET complication, which can be life-threatening! In the case of ET, both arterial (e.g. ischaemic stroke or cerebral infarction, myocardial infarction) as well as deep vein thrombosis (e.g. pulmonary artery thromboembolism) may occur. The risk of thrombosis is higher in older patients and in patients with concurrent diseases, prior thrombosis and a high number of platelets. Thrombosis may also occur in the case of a slightly increased number of platelets.
- Haemorrhages occur rarely and mostly in the case of very high platelet counts (>1000 ~ 109/L). Haemorrhage may manifest as prolonged or abundant bleeding from a small wound, frequent and abundant nosebleeds, haemorrhaging gums or menstruation with a lot of blood.
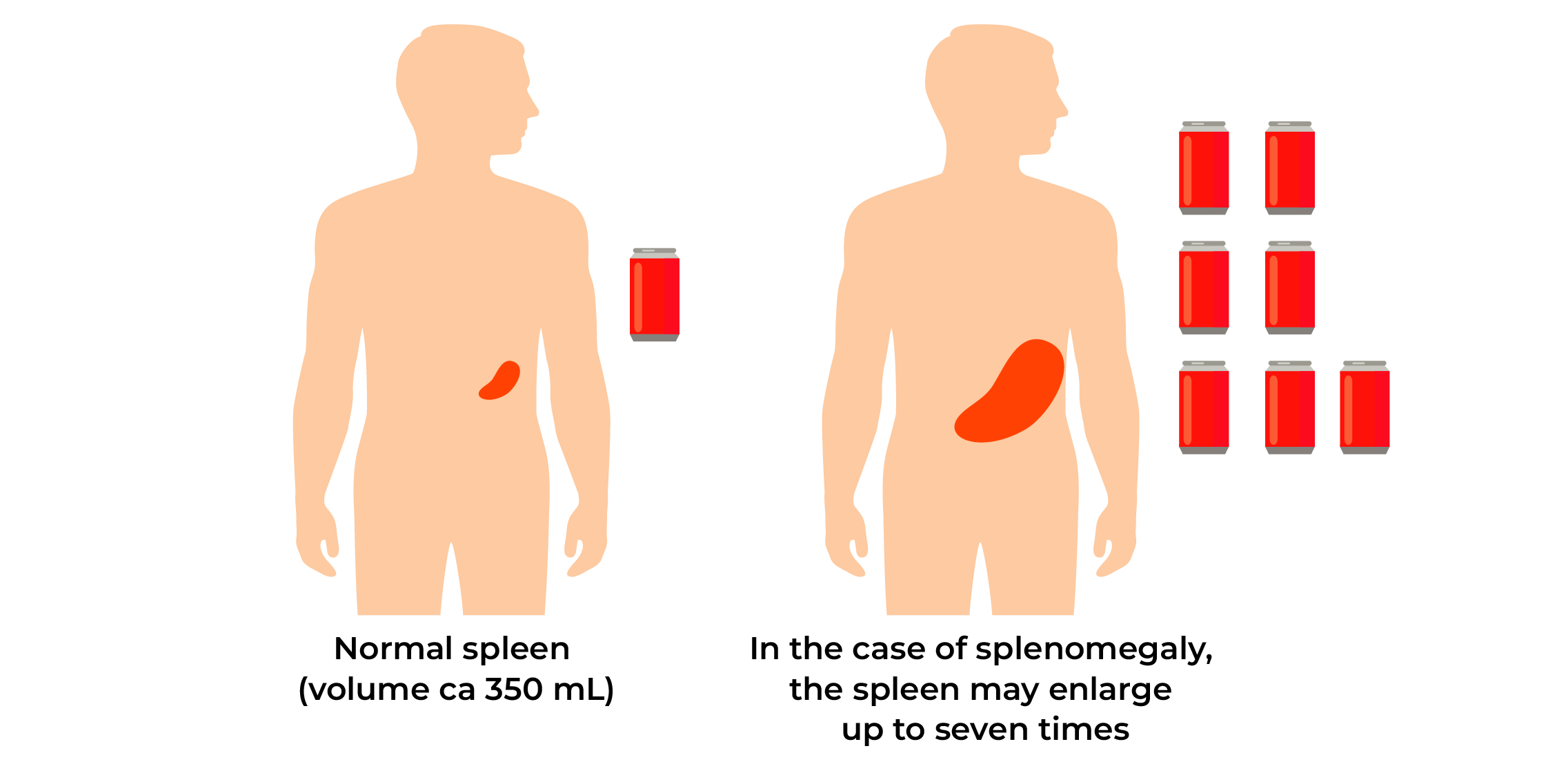
- Enlarged spleen or splenomegaly occurs in 30-50% of patients and may cause feelings of discomfort and fullness, rarely also pain in the upper left abdomen.
- General symptoms such as tiredness, weakness, skin itching, sweating and low fever may occur.
Diagnosis
Often, the disease is found accidentally when there is a higher than normal number of platelets (≥450 x 109/L) persisting for at least two months and other causes of increased platelet count are excluded. Values of other blood parameters – leukocytes, haemoglobin, haematocrit and erythrocytes – may be normal. For diagnosis confirmation, bone marrow samples should be taken with proliferation of megakaryocytes (progenitors of platelets) for ET. Enlarged spleen may be felt during abdominal palpation.
Treatment
ET is a chronic disease that cannot be cured. In treatment planning, disease symptoms and thrombosis risk are evaluated. Patient without symptoms and disease signs and low thrombosis risk may simply be monitored. In patients with high risk of complications (e.g. prior thrombosis, age over 60, cardiovascular diseases or their risk factors, etc.), the main treatment aim is to reduce the number of platelets. This reduces thrombosis risk. For thrombosis prevention, lifestyle risk factors should be minimised (stopping smoking, reducing weight, keeping blood pressure within normal limits, exercising regularly).
Medicinal products used
- Low-dose aspirin (so-called baby aspirin) is used to reduce the risk of platelet aggregation and thrombosis. Aspirin may irritate gastric mucosa causing gastric discomfort, nausea and pain. Anticoagulant therapy (blood coagulation inhibiting therapy) has to be prescribed when the risk of thrombosis is very high due to concurrent diseases.
- Hydroxycarbamide or hydroxyurea is a chemotherapeutic agent suppressing cell production in bone marrow and the most often used drug for ET. Hydroxycarbamide effectively inhibits the maturation and division of haematopoietic cells, therefore the number of erythrocytes and leukocytes may be reduced in addition to that of platelets. As the drug suppresses haematopoiesis, which may be accompanied by excess reduction in blood cells, regular checking of blood analysis results is very important. The therapeutic dose will be decided on the basis of blood test results. Hydroxycarbamide will be taken orally as capsules according to the regimen drawn up by the haematologist. Usually, hydroxycarbamide is well tolerated; there are few side effects and these are usually mild. Sometimes, the medicinal product may cause tiredness. Skin colour may become darker. There is a higher risk of developing skin tumours (avoid sunbathing). When ulcers develop on oral mucosa or legs during treatment with hydroxycarbamide, the attending doctor should be informed!
- Interferon-alpha is a substance usually produced in body cells to fight infections and tumour cells. This drug is preferred in younger people. Interferon-alpha reduces the number of platelets. The drug is injected subcutaneously according to the regimen prescribed by the doctor. The main side effects are flu-like symptoms, which manifest at treatment initiation: high fever, whole-body pain and malaise. Therefore, it is recommended to take paracetamol before the injection and to inject the drug in the evening before sleep. The side effects usually disappear with prolonged use.
- Anagrelide is used rarely: in cases when the patient doesn’t tolerate hydroxyurea and interferon-alpha and/or these drugs do not give the desired treatment result. Anagrelide slows the production of platelets in bone marrow. Possible adverse reactions are fluid retention, problems with blood pressure, headache, drowsiness, cardiac arrhythmia and diarrhoea.
Busulfan and radioactive phosphorus P32 are rarely used.
What the patient can do themselves
Maintain a normal weight and do regular physical activity (at least 30 minutes of walking every day). Avoid prolonged stress position, e.g. sitting (before travelling consult with a doctor). Consult with a haematologist when planning pregnancy and getting pregnant. Eat a healthy, balanced diet, avoid fatty foods. Keep blood pressure, cholesterol and blood glucose under control. Do not smoke.
Prognosis
Mean survival in patients with ET diagnosis is almost equal to that of the general population but depends largely on the treatment results of the specific patient and their age and concurrent diseases. With treatment, the disease is often stable for over ten years. Over the years, ET may progress to myelofibrosis and in 1-2% of patients to acute leukaemia.
In the case of myelofibrosis, bone marrow is gradually replaced by fibrotic tissue and less and less space is left for normal haematopoiesis. Blood cell production is partly transferred to the spleen, causing its enlargement. With time, the number of blood cells may reduce significantly, therefore patients sometimes become dependent on transfusions of blood components. In the case of acute leukaemia, proliferation of blasts (immature tumorous cells) occurs, leading to a worse prognosis.
It is not possible to influence the course of ET as a disease, but it is possible to prevent complications caused by the disease by following the doctor’s recommendations exactly and leading a healthy life.
Compiled by: Dr Marge Rahu, Dr Halliki Kõdar, Dr Maris Pärnat, Dr Kreete Ilves and Dr Mirja Varik, members of the Myeloproliferative Neoplasms Working Group of the Estonian Society of Haematologists

