CLL or chronic lymphocytic leukaemia (previously also termed chronic lymphoid leukaemia) is a malignant tumour of the haematopoietic tissue, where the cancer mainly attacks the lymphatic system but also accumulates in the blood, bone marrow and spleen.
What disease this is?
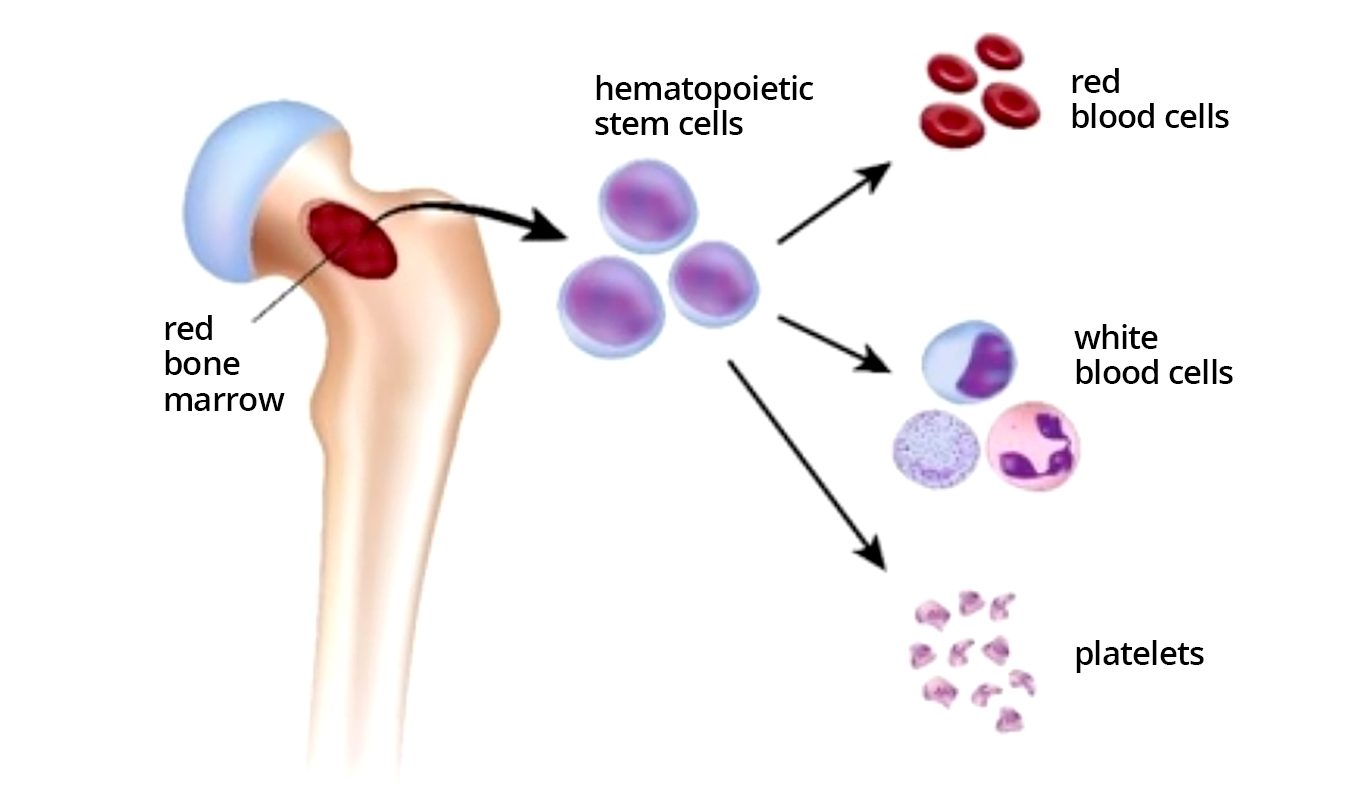
Chronic lymphocytic leukaemia (CLL) is a type of blood cancer. This tumour develops from lymphocytes. Lymphocytes are white blood cells circulating in the blood, the task of which is to protect the body against pathogens. Lymphocytes which have changed because of the tumour cannot complete this task. This is the main reason CLL patients become ill more easily and recovery from common viral or bacterial diseases is more difficult.
The word ‘chronic’ means that the disease course is slower than with acute leukaemia.
CLL is mainly a disease of elderly people. Average age at diagnosis is ca 70 years. People under 40 become ill very rarely. Approximately 100 persons per year receive a primary diagnosis in Estonia.
CLL is not a contagious disease; it will not spread from human to human or from animal to human. CLL is not a hereditary disease. Nonetheless, familiar disposition to different haematopoietic diseases has been observed.
Symptoms
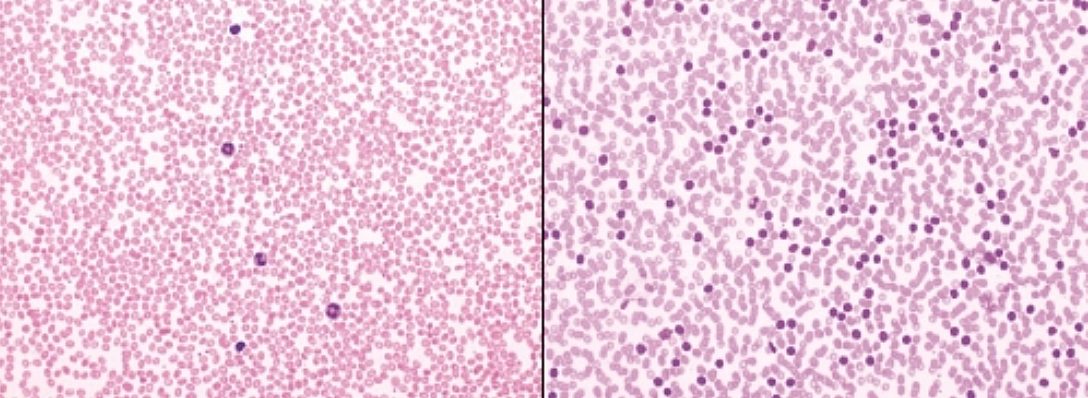
Many, even most, patients have no specific health complaints at the time of CLL diagnosis. The doctor becomes suspicious of the disease when looking at blood analysis results. The blood analysis may have been done for another disease or during a prophylactic check-up. Increased total count of white blood cells and increased percentage of lymphocytes are the key characteristics.
If there are complaints, they may be as follows:
- Enlarged but painless lymph nodes in neck, armpit or groin
- Unusual heavy tiredness
- Unexplained fevers for a couple of months
- Heavy night-time sweating requiring a change of clothes
- Unintentional weight loss
- Frequent infections in recent months
If you have these signs, see a doctor. None of these are unique to CCL but may occur in the case of many other diseases. Further investigations are required.
Causes
The causes of CLL are not clear. It is known that gene mutations occur in haematopoietic cells throughout life; therefore, abnormal ‘non-operational’ lymphocytes are formed. In addition to a deficient ability to operate, CLL lymphocytes also have a longer lifespan than healthy cells. They start to accumulate in the body and oust normal haematopoiesis.
Scientific research to determine the causes of CLL is very actively performed in many labs around the world.
What factors can influence morbidity?
- The probability of becoming ill increases with age.
- Men have higher probability of becoming ill.
- Caucasians become ill most often; Asians rarely have this disease.
- Family history of blood cancer. The probability of becoming ill is higher when close relatives have been diagnosed with CLL or another haematopoietic tumour.
- Exposure to certain pesticides and insecticides can increase the risk of CLL.
Complications
With CLL, the situation may worsen in the following circumstances:
- Autoimmune complications.
- In up to 25% of patients, a situation occurs when, due to disturbances in the operation of the immune system, the patient’s own immune system starts to attack red blood cells and/or platelets.
- Transformation or change into a more aggressive tumour.
- In a small percentage of CLL patients, the disease may transform into a more aggressive tumour – diffuse large B-cell lymphoma. Such transformation is called Richter’s syndrome.
- Frequent infections.
- Above all, CLL patients may frequently have common respiratory infections (pharyngitis, bronchitis, pneumonia). At times, more severe infections occur.
- Becoming ill with other tumours.
- CLL patients have a higher probability of becoming ill with other tumours (for example, bladder, lung, gastric or throat cancer).
Analyses and investigations
Diagnosis
A venous blood test is sufficient for diagnosing CCL.
- Counting and characterising blood cells or a clinical blood analysis allows the determination of a higher than normal lymphocyte content in the blood, which may be a sign of CLL. A clinical blood analysis is available at each level, including at a general practitioner. When a blood disease is suspected, the patient is referred to a haematologist’s appointment.
- Determination of lymphocyte type. The test is called flow cytometric immunophenotyping and it lets us know if the lymphocyte count has increased due to CLL or another haematopoietic tumour or due to an infection. Immunophenotyping is a very accurate and specific method requiring special training and equipment. The test is ordered and interpreted by specialist doctors/haematologists and it can only be done in the laboratories of Tartu University Hospital or the North Estonia Medical Centre.
Determination of risk group
Assessment of CLL prognosis or determination of risk group has been an object of interest for doctors and scientists for decades. Tens of laboratory-measurable indicators have been analysed during this time. Now, those that remain really have an impact on treatment decisions and thus on treatment results. As a rule, investigations for evaluating prognosis are not done upon diagnosis but when treatment initiation is required.
- Determination of genetic aberrations of lymphocytes. A cytogenetic test FISH (fluorescence in situ hybridization) allows the evaluation of certain chromosomes and their changes in lymphocytes. Changes del17p/TP53 and del11q found in tumour cells indicate high risk.
- Other genetic investigations
- Changes in karyotype or all chromosomes are more widely evaluated with a conventional cytogenetic test. Changes in three or more chromosomes are a sign of high risk.
- IInvestigation of mutations in the immunoglobulin heavy chain variable region (IGHV) is a method that is important in evaluating disease prognosis and choosing treatment options. Non-mutated IGHV is a high risk indicator.
Sometimes, the doctor considers the following investigations necessary:
- Bone marrow aspiration and trephine biopsy
- Computer tomography
- Lymph node biopsy
All methods required for CLL diagnosis and prognosis evaluation are available in Estonia.
Determination of stage
When the diagnosis has been confirmed, the doctor evaluates the amount of the disease in the body or the stage. Stage determination is a prerequisite for making a treatment decision.
Determination of blood cancer stage is different from solid tumours. Here, terms like metastases are not used because the nature of haematopoietic tumours (includingCLL) is systemic, i.e. they are whole body diseases. For CLL, since the 1970s, two stage classifications based solely on clinical indicators have been used, according to the classifications of authors Rai and Binet, which both differentiate early, intermediate and advanced stages.
In addition to the old classification, new risk scores have been used in recent years, which to a great extent are based on genetic prognosis markers or the biological nature of the disease.
Treatment
CLL is a disease with a chronic course and it is not yet known how to cure patients completely. The aim of treatment is to achieve a treatment response lasting as long as possible or improving/maintaining quality of life.
The time of treatment initiation depends on the disease stage and the presence of general symptoms.
The choice of medicinal product/treatment regimen depends on the patient’s age, general health status and the biological nature of the disease or risk group as well as treatment funding or financial availability.
As in the case of other malignant tumours, treatment decisions are made by the council of specialist doctors following international recommendations or treatment guidelines. CLL treatment is carried out by a specialist doctor/haematologist.
In early stages, treatment is not needed. This information is often unanticipated by the patients because in the case of tumours rapid treatment initiation is more common. The justification for this proceeds from clinical research studies. It has been proven that treatment started too early, i.e. when the disease doesn’t worsen the patient’s condition, does not prolong the patient’s life but introduces treatment-associated risks which are not justified at that moment. During the early stage of the disease, the patient will be actively monitored by a haematologist. This means that the doctor prescribes regular check-up appointments with an interval of a couple of months. This approach is called ‘watch and wait’. Waiting does not make the disease less susceptible to treatment. A third of all patients will never need CLL treatment.
In intermediate and advanced stages, the disease needs treatment in most cases. Choice of treatment has become markedly better over the years.
- Chemotherapy – fludarabine, cyclophosphamide, bendamustine, chlorambucil. Chemotherapy agents destroy the tumour preferentially but also damage normal body cells. Treatment can be performed intravenously or tablets may be used. Depending on the situation, one preparation or a combination of several medicinal products can be used. Common side effects during the treatment are tiredness, temporary reduction of blood cells and higher infection risk. Treatment is usually performed in courses, with time for recovery in between. Chemotherapeutics used in CLL treatment usually do not cause alopecia. Chemotherapy is the oldest treatment method, the percentage of which has reduced due to new drugs.
- Biological treatment. These ‘smart’ drugs have been developed to distinguish tumour cells from normal cells. There are special proteins on the surface of CLL cells that can be used as targets. Biological drugs or monoclonal antibodies bind to these proteins and destroy the tumour cell. At the moment, two drugs belonging to this group – rituximab and obinutuzumab – are used in the treatment of CLL. Common side effects are fever and chills upon treatment initiation and high infection risk during or after treatment courses. Biological drugs are mostly used in combination with chemotherapy, which in such cases is called immunochemotherapy.
- Immunochemotherapy is still the most used treatment option. There are several options. A fludarabine/cyclophosphamide/rituximab combination is suitable for younger patients with a good health status and may result in a period without disease signs lasting for more than ten years. A bendamustine/rituximab combination also yields long-lasting remission, causing less toxic side effects at the same time. An obinutuzumab/chlorambucil combination is effective but more sparing and therefore the best choice for elderly patients with concomitant diseases.
- New drugs – ibrutinib, venetoclax – which are called targeted therapies, act via completely different mechanisms of action than the medicinal products used until now. They are able to interfere with the life cycle of tumour cells without significantly damaging other body cells. New drugs are able to destroy those cancer cells that chemotherapy cannot.
- Allogeneic transplantation of haematopoietic stem cells (collected from a donor). In this treatment method, very strong chemotherapy is used that destroys the patient’s haematopoiesis. The haematopoietic cells or stem cells of a healthy person are then administered intravenously to the patient; the cells find their way to the bone marrow, start to multiply there and normal haematopoiesis is restored. Transplantation experience is prolonged, ca 40% of patients who undergo transplantation achieve a good treatment result. The main shortcoming of this method is toxicity, but its percentage has reduced with the introduction of new drugs.
- Cellular therapy is developing rapidly with promising results.
Clinical studies
Clinical drug studies test new drugs and different combinations or new timings of existing drugs. It must be kept in mind that participation in a clinical drug study can give a patient an additional option for influencing the disease but gives no guarantee of improvement. Ask your doctor if there is a drug study suitable for you.
Some examples of questions whose answers scientists around the world are trying to find:
Can a cure be achieved?
What are the best drug combinations for the treatment of high-risk patients?
What can I do to help myself?
- Try to avoid infections. CLL patients have a tendency to get different infections. Vaccination against flu is recommended during each season. Avoid contact with sick persons. Wash hands often and scrupulously.
- Try to keep your body strong. Eat a varied diet, including lots of different vegetables. There are lots of references on the beneficial effect of green tea in scientific literature. Sleep enough. Move around in fresh air every day. Keep you other chronic diseases (for example, diabetes, heart and lung diseases) under good control.
- Reduce the risk of developing other tumours. CLL patients have a tendency to get other tumours. Do not smoke. Drink a little/moderate amount of alcohol. Eat lots of fruits and vegetables. Avoid intense sunbathing and use sun cream.
- Visit the doctor at the preassigned times. Blood analyses and examinations done with sufficient frequency help to evaluate whether the disease is progressing. A feeling of anxiety before the visit is natural; don’t avoid the visit. Invite a family member or a friend to accompany you if it gives you support.
Alternative Medicine
No alternative medicine remedy will cure CLL,but you may get help to alleviate a symptom or treatment side effect.
CLL patients often feel tiredness that is little influenced by drugs. It is possible that moderate physical exercise, meditation, relaxation techniques and yoga have a positive impact on you.
Attention! Various allegedly immune-stimulating or direct anti-cancer liquids, tablets, etc. (even if brought from far-away lands and very expensive) do not have a scientifically proven beneficial effect in CLL treatment. More importantly, their damaging effect is not excluded.
Tell your doctor about your choices.
Psychological support
CLL is mostly a slowly developing tumour that doesn’t need treatment at all in many cases. Nonetheless, it is a malignant disease and learning about it causes shock or severe anxiety.
Over time, you will adapt to this situation and learn to live with your disease.
In this process, you will likely find help if you:
- Learn more about your disease. Ask your doctor and write down your questions before the doctor’s visit, if needed. A lot of information about this Contact other cancer patients, but don’t compare yourself directly to anyone. There are many types of blood cancer; even within the limits of the same diagnosis, individual differences are big. Eesti leukeemia- ja lümfoomihaigete liit is active in Estonia.
- Rely on your friends and family. Talking about the diagnosis may be difficult and listeners will likely react very differently. Nonetheless, you will feel better when you are able to talk with others about your disease. There may be more people offering help. Think about from whom and what kind of help (domestic work, transport, listening, company) you need.
- Seek professional psychological help, if required.
1 Tervise Arengu Instituut. PK10: Pahaloomuliste kasvajate esmasjuhud paikme, soo ja vanuserühma järgi.
Compiled by: Dr Iige Viigimaa
Last updated: 06/2021

