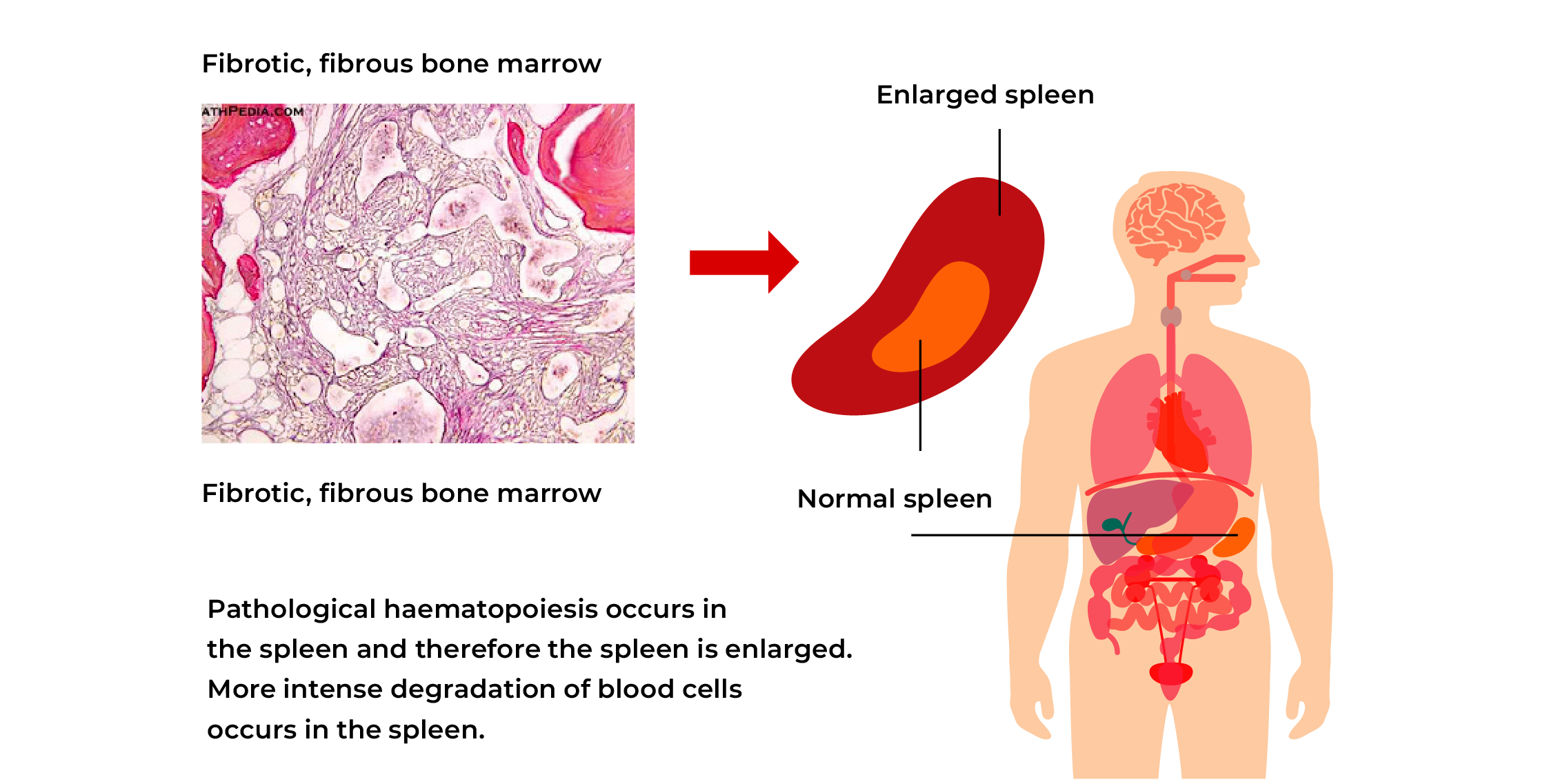
Myelofibrosis (MF) is a tumorous bone marrow disease belonging to the group of myeloproliferative diseases. This is a chronic disease where an abnormally large amount of fibrosis (fibrotic scar tissue) develops in the bone marrow, therefore the amount of bone marrow producing blood cells normally is reduced. MF may develop spontaneously (primary myelofibrosis) or in a patient who has been previously diagnosed with another bone marrow disease (e.g. polycythaemia vera or essential thrombocythemia). Treatment does not depend on how the disease has developed.
MF is a rare disease. An average of 1.5 cases per 100,000 people per year are diagnosed. Blood analyses, histological investigation of bone marrow and abdominal ultrasound investigation are the bases for diagnosis.
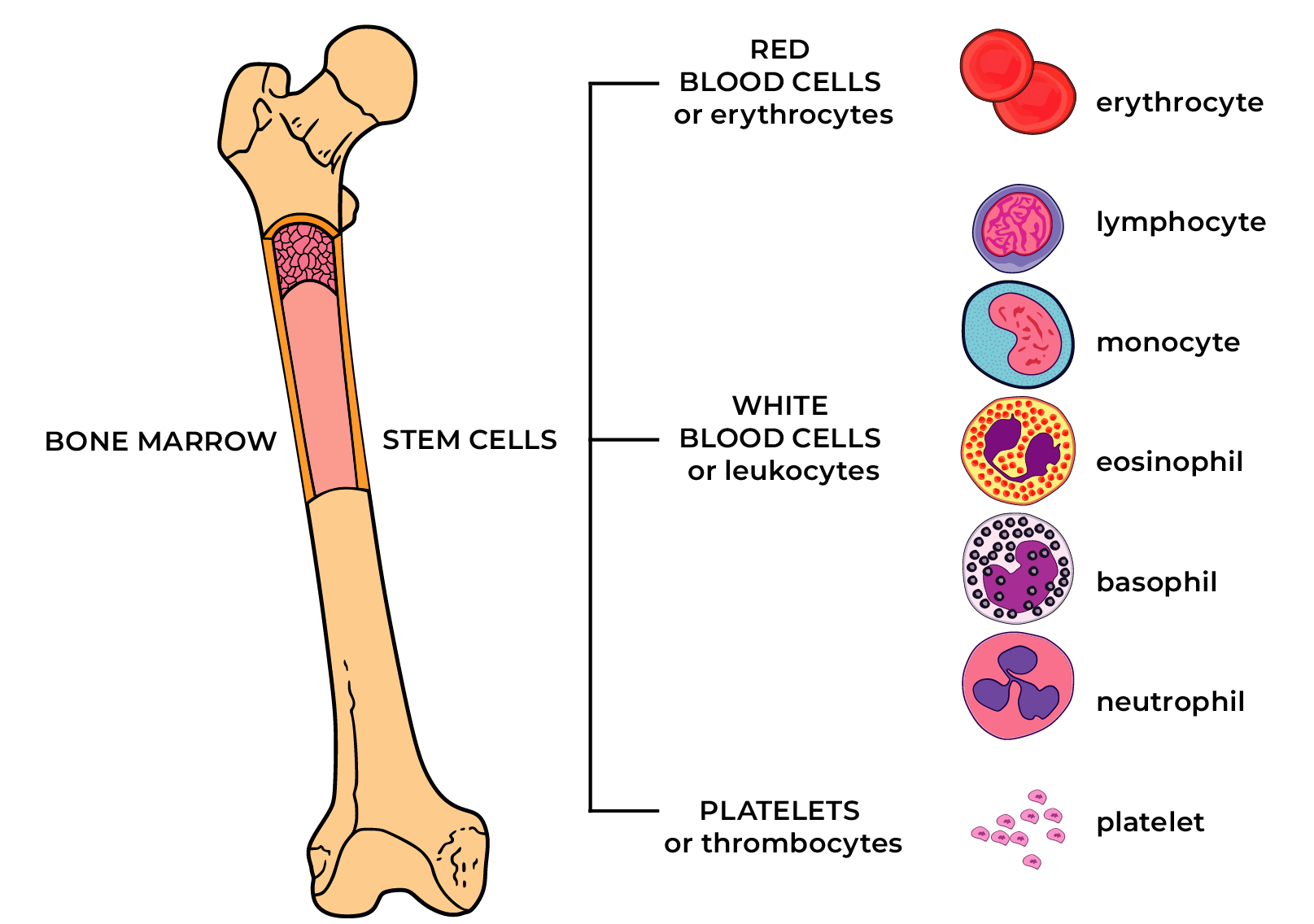
MF is caused by a change in bone marrow stem cells. Recently, scientists have discovered DNA changes leading to impaired haematopoiesis regulation and production of certain cells in larger quantities than the body needs.
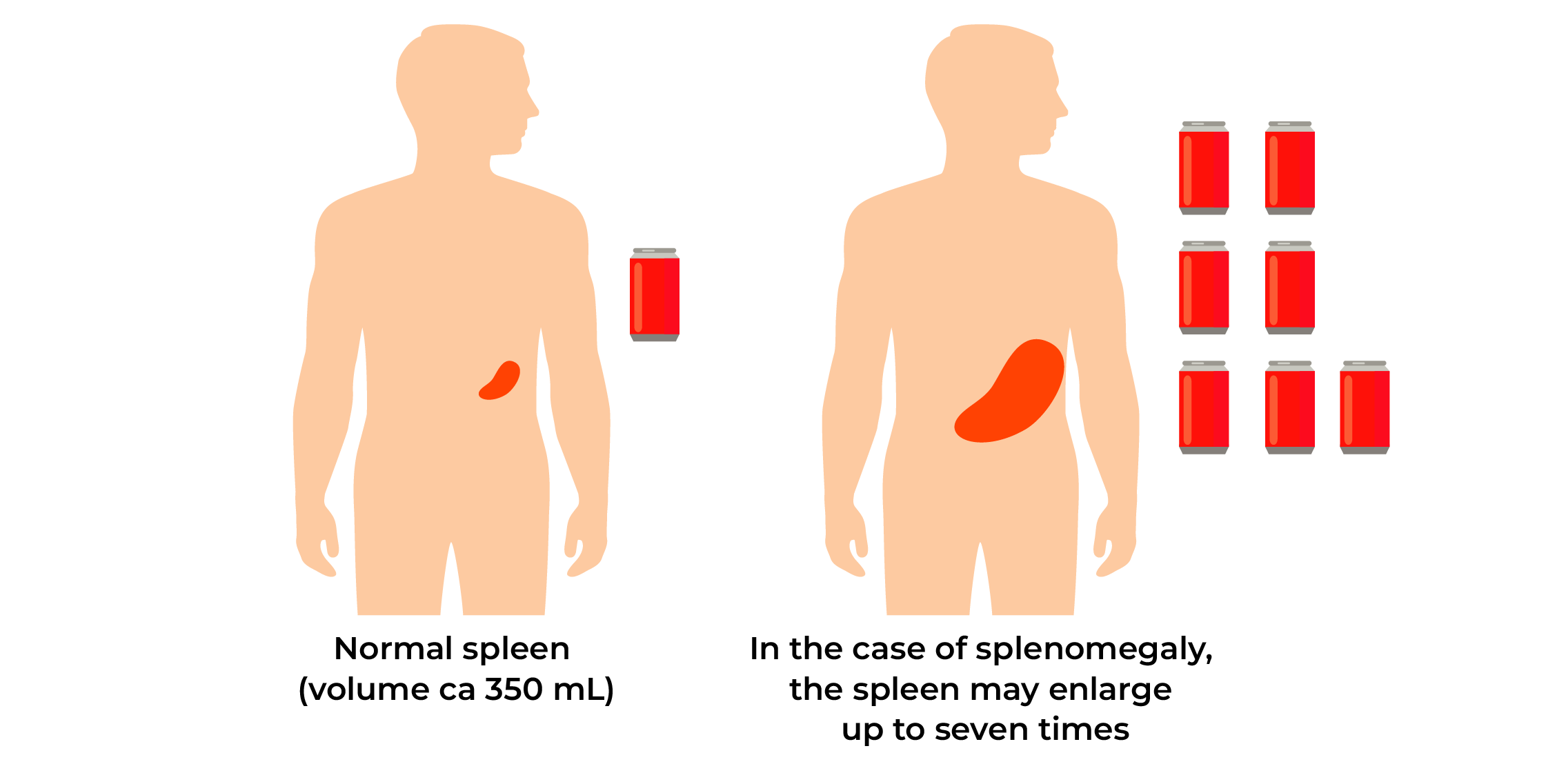
As a result, bone marrow fibrosis occurs and the production of normal blood cells is reduced. Anaemia develops gradually; platelet and leukocyte values may become low. The spleen and liver may make a compensatory take over of the production of blood cells; their enlargement may cause complaints.
Most often, in ca 60% of cases, a change is found in the Janus-kinase 2 gene (JAK2) and in ca 30% of cases in the calreticulin gene (CALR). Less often, a change is found in the MPL gene with a similar mechanism of action.
The cause of these genetic changes is unknown. Possible risk factors include exposure to chemicals and ionising radiation.
Myelofibrosis is not a hereditary disease and it is not possible to prevent it!
Symptoms
MF is mostly diagnosed because of the patient’s complaints, but sometimes accidentally found changes in blood parameters lead to diagnosis.
Common complaints are:
- tiredness, weakness, dyspnoea, breathlessness, palpitations, pallor due to anaemia;
- due to spleen (and liver) enlargement, upper abdominal pain, feeling of fullness, weight loss;
- general symptoms such as increased nocturnal sweating, fever, skin itching;
- frequent infections due to shortage of white blood cells; and
- bone and joint pain.
In 12-25% of patients, the disease may develop into acute myeloid leukaemia.
Treatment
The objective of MF treatment is the alleviation of symptoms, the improvement of quality of life and the prolongation of survival, if possible.
Treatment is initiated when symptoms appear. The MPN-SAF TSS questionnaire obtained from the doctor or nurse helps to evaluate the symptoms.
Patients without disease symptoms, for example, spleen enlargement, severe anaemia or other complications, may not need treatment. A stable condition may last for years, but the patient needs a regular health assessment by a haematologist. Studies have not proven that initiation of treatment before the appearance of symptoms improves prognosis.
At the moment, there are no drugs that cure the disease. Transplantation of bone marrow stem cells from another person (allogeneic) is the only treatment method that potentially cures myelofibrosis, but it can be performed only in younger patients without significant concurrent diseases. Thus, stem cell transplant is suitable for less than 5% of MF patients.
Treatment options
Medicinal products used
JAK-inhibitors are a group of medicines targeting and inhibiting the activity of the intracellular JAK-STAT signal pathway causing myelofibrosis. These medicines help to effectively reduce spleen size and general symptoms and may prolong survival.
Due to the mechanism of action of the drugs, anaemia may worsen and platelet number may decrease at the onset of treatment. Other frequent side effects include headache and dizziness, haemorrhage, infections. Treatment should not be stopped abruptly as disease symptoms may recur rapidly.
In chemotherapy, anti-tumour (cytotoxic) agents are used to destroy tumour cells. This treatment method can be used in MF treatment, especially in the case of severe symptoms. Chemotherapy may help to reduce spleen and liver size, to control other symptoms. Chemotherapy may not be suitable for everyone.
Hydroxyurea or hydroxycarbamide is the most often and in most cases first used chemotherapeutic agent to reduce spleen size and other disease symptoms. Hydroxyurea is taken as capsules every day at home. The medicinal product is usually well tolerated. Decrease in blood cell counts, skin rash, leg ulcers, nausea and diarrhoea may occur as side effects.
Interferon-alpha is used to treat MF in younger patients. The medicinal product is similar to the substance produced in the body cells to fight infections and tumorous cells. Interferon-alpha is mostly used in MF patients with an enlarged spleen, bone pain and a high platelet count.
Removal of spleen
Surgical removal of the spleen is considered when other treatment options to reduce symptoms caused by spleen enlargement have not helped and there are no contraindications to surgery.
Expected benefit of surgery: reduction of symptoms, reduction of pressure in vein entering the liver, less need for blood transfusions.
Risks: infections, liver enlargement, platelet count increase, thrombosis risk, complications associated directly with surgery.
Anaemia treatment
- Periodic transfusions of red blood cells reduce symptoms caused by anaemia. As a result of copious blood transfusions, chronic iron overload may develop in the body – excess iron accumulates in the body, damaging the heart and liver. Removal of excess iron may require the use of a special medicinal product.
- Erythropoietin (EPO) may be used to increase haemoglobin level in the case of anaemia. Medicines of this group are administered as subcutaneous injections usually once a week. Treatment results are better in patients with a low serum EPO level and who are not dependent on blood transfusions. More common side effects include pain at the injection site, increase in blood pressure and increased thrombosis risk.
- Hormone treatment with glucocorticoids is used above all in the case of anaemia caused by autoimmune haemolysis (when the body produces antibodies against its own red blood cells), but this may also help to increase haemoglobin level in the case of non-haemolytic anaemia. Hormone treatment is also used in combination with some other drugs. More common side effects include nausea, heartburn, headache, sleep disorders, osteoporosis.
Radiotherapy
Low-dose radiotherapy is used to reduce spleen volume when other treatment methods have not yielded the desired results. Radiotherapy may increase infection risk. The effect of this treatment method is temporary, lasting mostly up to half a year.
Prognosis
No stages are identified in MF. Survival prognosis is assessed individually for each patient. Depending on age, blood analysis results and general symptoms, patients are divided into risk groups (risk evaluation scales IPSS and DIPSS). Sometimes, the need for blood transfusions and changes in cell chromosomes are taken into consideration when determining the risk (risk evaluation scale DIPPS plus). Treatment and prognosis both depend on the risk group. The course of the disease differs; predicted life expectancy with the disease may vary from several years to >10 years. Treatment outcomes are individual and not predictable.
Compiled by: Dr Marge Rahu, Dr Halliki Kõdar, Dr Maris Pärnat, Dr Kreete Ilves and Dr Mirja Varik, members of the Myeloproliferative Neoplasms Working Group of the Estonian Society of Haematologists

